What:
Participating in screening means that you have no symptoms. You have no bleeding. You have no abdominal pain, weight loss, change in bowel habit. You have no risk factors for colon cancer that would usually require a colonoscopy (i.e., strong family history of colon cancer, inflammatory bowel disease). If you have these issues, you should see your GP or get in touch for an appointment.
Why:
Each year between about 2500 and 3000 New Zealanders will be diagnosed with colorectal cancer and between 1100 and 1200 will die as a result of colorectal cancer. This represents both the second most common cancer diagnosed and cause of cancer death. Absolute rates continue to rise in the face of an aging and increasing population.
This is also a big problem world-wide. There are over one million new cases of colorectal cancer diagnosed world-wide each year and 600,000 deaths. In addition, NZ has the lowest percentage of surgically curable localised disease (28%) when compared with Australia (34%), America (40%) and the United Kingdom (42%). 20% of disease at diagnosis is metastatic (i.e., incurable and spread elsewhere in the body).
We know that most colorectal cancers develop from precancerous polyps. Polyps are like warty outgrowths that form in the lining of the colon. Removing these can help to remove the risk of developing colon cancer. Studies have shown that regular screening for and removal of polyps reduces your risk of developing colorectal cancer by up to 89% with colonoscopy. Similarly, if a cancer is found, it may be treated, hopefully at an earlier stage than it would have been found otherwise
When polyps are small and growing, you will not have any symptoms. It is only when they grow very large that these may bleed, cause pain, or change your stool habit. This is why screening is important.
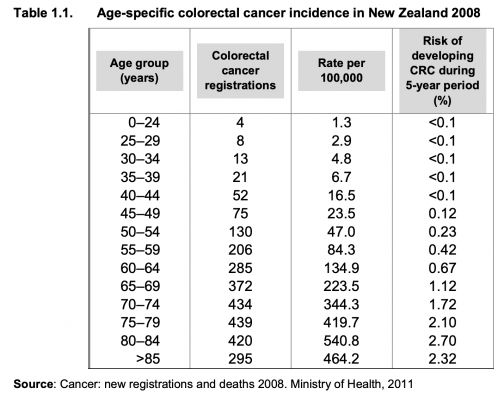
In Western societies, approximately 5% of the population will develop CRC in their lifetime and up to 2.5% will die of the disease
How?
The best test for screening is performing a colonoscopy, as this is a direct examination of the bowel. If you are between 60 and 74 and in a participating centre in New Zealand, you will be sent a stool test in the mail. This is checking for microscopic blood. If microscopic blood is present, you will be asked to have a colonoscopy.
Ages to start screening is different in other countries:
- Netherlands: 55
- Australia: 55
- Scotland: 50
- Japan: 40 years old.
Within New Zealand’s bowel screening programme, a positive result is triggered if the blood (haemoglobin (Hb)) found in a sample is over 200 nanograms of Hb in a millilitre of buffer. The bowel screening pilot found that for readings at this level, for every 100 people we know that approximately eight will have a cancer found in the first round of screening. For every 100 people with FIT results below the threshold there will be very few cancers found. The bowel screening pilot found that readings at this level and higher accounted for 80 percent of bowel cancers found and therefore indicated a higher likelihood of bowel cancer (5)
False positive test results can occur
False positive results can occur too where screening test results may appear to be abnormal even though no cancer is present.
A negative screening result
This means blood has not been detected in your sample, and it is recommended that you repeat a bowel screening test every two years. A negative result does not mean that you do not have, or can never develop, bowel cancer because some bowel cancers do not bleed, or bleed on and off. A person who receives a false-negative test result (one that shows there is no cancer when there really is) should still seek medical attention.
_______________________________________________________________________________
ADVANCED information
With the understanding of the adenoma to carcinoma sequence (Figure 1), CRC is highly amendable to screening, and after more than 50 years of data analysis, quality evidence exists to demonstrate its efficacy, which is estimated to be about 25–50 per cent in preventing disease-specific death.
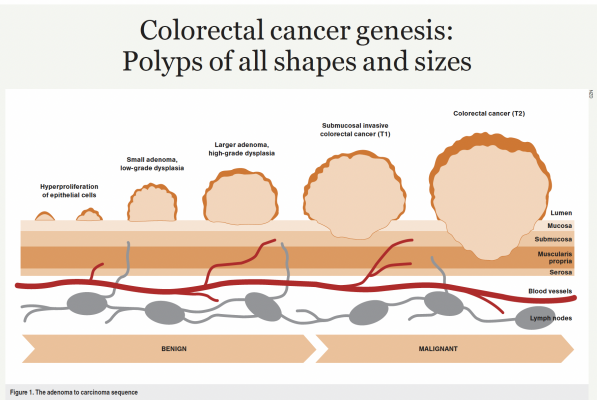
It has been suggested that it could be labelled “colorectal neoplasia screening” as it targets both cancer precursors (polyps) and early cancers to decrease CRC incidence and mortality. The stage of cancer at diagnosis is the most important determinant of prognosis. The five-year survival rate for stage I CRC is 91 per cent, dropping to 72 per cent for locally advanced disease and 14 per cent for stage IV. Studies demonstrate a 4–6 per cent increase in stage I CRC diagnosis with the onset of screening.
On this basis, New Zealand started a bowel screening pilot in Waitematā in 2011, which was then rolled out to the rest of the country in a staged fashion starting in 2017, with all eligible New Zealand centres now performing screening.
Screening in New Zealand is performed via faecal immunochemical test (FIT) to detect microscopic blood in the stool. A test kit, instructions and consent form are received in the mail, then the sample is collected and sent back in a zip-lock bag.
In the pilot, the threshold of 75ng/ml was used to define a positive test. Many countries use a cutoff of 75ng/ml or 100ng/ml, including Australia. However, the New Zealand threshold has been increased to 200ng/ml in the current nationwide programme, largely due to workforce and resource constraints. In the pilot study, 17 per cent of the cancers detected occurred in participants with a FIT result of 75–199ng/ml. It is important to recognise this as patients may be falsely reassured by a reported “negative” test, thinking there is no evidence of bleeding in the stool, but it does not report an absolute numerical value. If abdominal symptoms develop despite a negative FIT result, CRC should remain as a consideration in the differential diagnosis.
The eligible age range during the pilot was 50–74 years, but this has been raised to 60–74 years, where approximately 40 per cent of CRC cancers are diagnosed. However, 30 per cent of CRC is diagnosed under the screening age, with nearly one-third of patients in this age group having stage IV metastatic disease. This age cutoff is also controversial, given that in May 2018, the American Cancer Society published guidelines recommending CRC screening start at age 45, and in Australia, GPs can offer a FIT starting at age 45. Austria and Japan recommend starting screening from age 40.
After some robust discussion and lobbying, the screening age for Māori and Pacific patients has been decreased to start at age 50, in an attempt to capture the 22 per cent of Māori aged 50–59 who are diagnosed with CRC.
Despite some potential deficits, screening has already been highly effective in New Zealand. In the first pilot only in Waitematā, 427 patients were diagnosed with CRC. Screening has also been shown to be cost effective, driven by considerable cost savings from avoided CRC treatments. Average levels of cost per quality-adjusted life year (QALY) for medications funded by Pharmac are in the range of $16,000 to $45,000. In comparison, a cost of less than $1000 per QALY makes bowel screening highly cost effective.
Increasing participation rates, which in the first New Zealand pilot was only 58 per cent of those invited, increases both efficacy and cost effectiveness. Although the cost of screening increases with increased participation rates, the cost offsets increase at a greater rate, which leads to an increase in net savings.
Any screening programme must align with resources and circumstances and take into account the broader health context to maximise a finite healthcare resource. CRC screening touches on fundamental issues of autonomy versus paternalism, informed decision-making, individual responsibility, choice, reason versus emotion, shared risk, delayed benefit, access to care, and social equity.
________________________________________________________________________________
Article on missed cancers with screening in NZ
Additional Information:
Ministry of Health National Bowel Cancer Screening Information:
Bowel Cancer Screening New Zealand:
https://bowelcancernz.org.nz/about-bowel-cancer/early-detection-and-prevention/screening/
Time to screen New Zealand:
https://www.timetoscreen.nz/bowel-screening/
Large published study on effectiveness of colon cancer screening:
